Release date: 2015-10-23
Congenital heart disease is the leading cause of death in newborns, with an incidence of about 4-13/1000. Fetal echocardiography (FECG) is the only method for prenatal diagnosis of fetal heart disease. Affected by the position and special circulation of the fetus, some cut surfaces that are easily accessible to adults are often difficult to display in the fetus, making FECG difficult and has not been widely used.
Compared with adults, the sternal and rib ossification of the fetus in the middle pregnancy is not obvious, and there is no lung interference. As long as the spine is avoided, we can observe the fetal heart structure from any position, that is, there may be a simpler The method is to complete the FECG.
The previous Israeli scholar Yagel recommended the use of five short-axis sections to complete the fetal heart ultrasound examination, which were the abdominal cross-section, the four-chamber view, the left ventricular outflow tract, the right ventricular outflow and the three-vessel tracheal section, which were subsequently Accepted by many experts. In 2013, the International Obstetrics and Gynecology Fetal Echocardiography Group published a consensus statement on what should be included in the fetal heart rate examination, which is basically consistent with Yagel's view. The author combined his own experience to analyze the method of continuous horizontal scanning of the fetal heart as follows.
Ultrasound technology
The fetal heart continuous transverse scanning technique starts from the transverse section of the fetal abdominal circumference, slides to the fetal head side to the four-chamber view, continues to slide or tilt the probe, and sequentially observes the left ventricular outflow tract section, the right ventricular outflow tract section, and the trivascular trachea. section. It is a method for systematically assessing the structure of the fetal heart. The tilting probe can obtain a longer outflow channel cut surface than the sliding probe to facilitate observation of the distal end of the outflow tract (Fig. 1), and even the entire ascending aorta can be observed; the right ventricular outflow tract is required to show the pulmonary artery branch.
The trivascular tracheal section also shows the transverse arch of the arterial catheter and the transverse arch of the aorta. It is the highest aspect of the fetal heart examination and is a difficult section to obtain. In the process of continuous lateral scanning, after the right ventricular outflow tract section is displayed, the probe continues to slide to the lateral side of the fetal artery to the transverse section of the arterial catheter, and the probe is rotated to the upper right side of the fetus until the transverse section of the arterial catheter is continuously displayed. The aortic transverse arch shows that the trivascular tracheal section can be obtained.
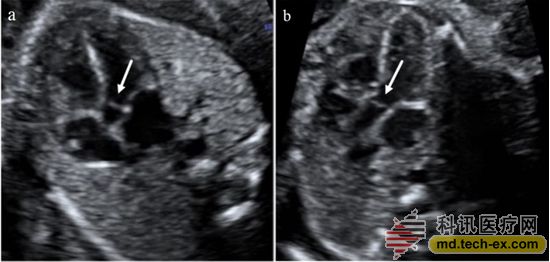
Figure 1: a and b are the left ventricular outflow tract cuts shown by the sliding and tilting probes, respectively, and the arrows show the aortic valve.
Compared with the tri-vascular tracheal section, the transverse approach of the arterial catheter and the aortic transverse arch are simple, and there is no need to rotate the probe. When the three-vessel tracheal section is not easy to display, the transverse arch of the catheter and the transverse arch of the aorta are evaluated one by one, which can replace the three blood vessels. The tracheal section was used to evaluate the structure of the large vessels. The coronary sinus section and the three-vessel section are also easy to obtain in the continuous scanning. The three-vessel section can be used as the extension section of the outflow section to evaluate the inner diameter and positional relationship of the large vessels. In short, the continuous horizontal scan of the fetal heart greatly simplifies the fetal heart examination technique. The difficulty of fetal heart ultrasound is no longer the acquisition of the facet, but the cognition of the facet. The observation of the facet is analyzed as follows.
Abdominal transverse section and four-chambered section
The fetal position is determined first during the examination. The transverse section of the abdominal cavity shows the left side of the cartilage, and the descending aorta is located to the left of the inferior vena cava (Fig. 2a). The four-chamber view should carefully evaluate each criterion rather than just counting the number of rooms. The heart is located on the left side of the carcass (Fig. 2b). The normal heart does not exceed one third of the chest area. Some cuts may have a small amount of hypoechoic wrap around the heart and are mistaken for pericardial effusion. An independent study suggests that this is usually a normal variation.
Under normal circumstances, the left axis of the mandrel is 45±20◦. Abnormal heart axes, especially when combined with outflow tract abnormalities, increase the risk of cardiac malformation. This finding may be related to chromosomal abnormalities. An abnormal position should be suspected when the heart and/or stomach of the fetus is not on the left side of the fetus. A sputum or a space-occupying disease, such as a cystic adenoma, can cause abnormal heart position. Abnormal heart position can also be secondary to lung dysplasia. The left axis of the mandrel can also be caused by abdominal fissure and umbilical bulging.
The normal fetal heart rate is 120-160/min. A transient bradycardia can be observed in the fetus during the second trimester. Sustained bradycardia, especially if the heart rate is below 110/min, you need to ask the fetal heart specialist to assess the possibility of heart block. Repeated heart rate reduction during late pregnancy may be caused by fetal hypoxia. Occasional leaks usually do not increase the risk of heart malformation, are generally benign and can heal themselves. However, in some cases there will be clinically significant arrhythmias, which is a testimony for fetal echocardiography. Multiple Doppler auscultations, targeted scans can be used to rule out effusions and to confirm normal fetal heart sections. A slight tachycardia can occur during fetal activity. However, persistent tachycardia (≥180 bpm) should consider the possibility of fetal hypoxia or more severe tachycardia.
Under normal circumstances, the two atrial cavities are similar in size, and the oval valve flutters in the left atrium. The lower interatrial septum, ie the primary interatrial septum, should be shown. It is part of the heart "cross" cross structure. The "cross" crossover structure consists of the lower part of the interatrial septum, the upper part of the interventricular septum, and the attachment point of the atrioventricular valve. It can be seen that the pulmonary veins flow into the left atrium, and at least two pulmonary veins are shown where the technique permits.
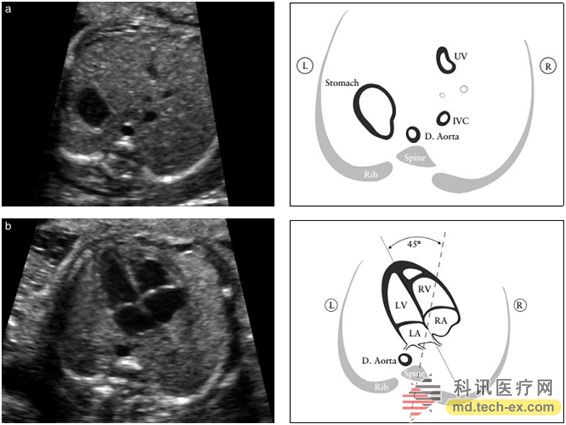
Figure 2 (a) determines its position in the fetal abdominal cross section. According to the position of the fetus in the uterus, the left and right sides of the fetus should be on the left side of the fetus. The descending aorta (D.Aorta) and the inferior vena cava (IVC) should be on the left and right sides of the spine respectively. The figure also shows a small umbilical cord. Venous (UV), (b) position of the heart and mandrel: the heart is mainly on the left. Compared with the axial position before and after the chest, the apex is 45±20° to the left.
The adjustment beam is a distinct muscle bundle across the right ventricular cavity that is close to the apex and helps to determine the morphological right ventricle. The apex of the left ventricle is smooth and forms the apex of the heart. The two ventricles should be similar in size and have no significant ventricular wall hypertrophy. Although under normal circumstances, there may be slight left and right ventricular asymmetry during late pregnancy, but the obvious left and right inconsistency during mid-pregnancy should be further examined. Left heart obstructive diseases, such as aortic stenosis and left ventricular dysplasia, are the main causes of this inconsistency.
Prenatal diagnosis of ventricular septal defect is difficult. When the ultrasound is parallel to the interventricular septum, the defect may be misdiagnosed due to "lost" artifacts. When the ultrasound system does not provide sufficient lateral resolution, especially if the size and position of the fetus are not satisfactory, the lack of a small chamber (1-2 mm) is often missed. It is therefore recommended that the sound beam be perpendicular to the interventricular septum at the interval between the examination rooms to avoid missed diagnosis or misdiagnosis. Although the diagnosis of ventricular deficiencies does not have much clinical significance in most cases, it may self-close in the uterus, but a small number of ventricular septal defects often have chromosomal abnormalities.
The two atrioventricular valves (the tricuspid valve on the right side and the mitral valve on the left side) should be open and closed freely. The attachment point of the tricuspid valve in the interventricular septum is closer to the apex (ie, normal displacement) than the mitral valve. Misplacement of atrioventricular valve is a key marker of atrioventricular septal defect.
Left ventricular outflow tract (LVOT) section
The left ventricular outflow tract shows that the aorta is emanating from the morphological left ventricle (Fig. 3), and the continuity between the anterior wall of the aorta and the ventricular septum, as well as the posterior wall of the aorta and the anterior mitral valve should be confirmed. The aortic valve is free to open and close, and the valve is not thickened. Tilting the probe to the cephalad can track the aorta to the aortic arch and the location of the three vessels. However, these vessels that recognize the aortic arch are not part of a routine cardiac exam. The left ventricular outflow tract section helps to detect the outflow tract septal defect and the conical arterial malformation that is not easily detected in the four-chamber view. For example, the tetralogy of the Fallot, the transposition of the great arteries, the double outlet of the right ventricle, and the permanent arterial trunk. A more independent exploration of the four-chamber view improves the detection rate of major cardiac malformations.
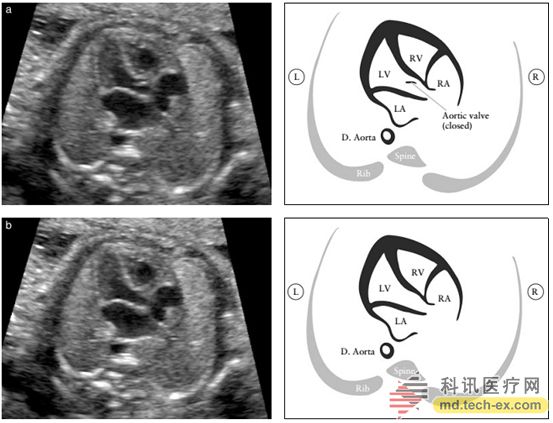
Figure 3 Left ventricular outflow tract (LVOT) section. This section shows the vessels connected to the left ventricle, and the continuity of the ventricular septum with the anterior wall of this large vessel is important. The aortic valve is not thick and open and close freely. Figure (a) shows the aortic valve closure and Figure (b) shows the aortic valve opening.
Right ventricular outflow tract (RVOT) section
The right ventricular outflow tract section shows the large blood vessels emanating from the morphological right ventricle (Fig. 4): the pulmonary artery is thus emitted and turned to the left rear of the descending aorta. It is usually slightly wider in the fetal period than in the aortic root, and the pulmonary artery crosses the descending aorta at a right angle immediately after it is emitted. At this level, as shown in Figure 5, the pulmonary artery is located to the left of the aorta and the superior vena cava is shown to the right of the aorta. The pulmonary valve is free to open and close, and the valve is not thickened. It is only when the branch of the blood vessel is seen that it is confirmed that the pulmonary artery is emitted from the right ventricle. The branch on the right is displayed first on the left. Branches are not always displayed due to the influence of fetal position.
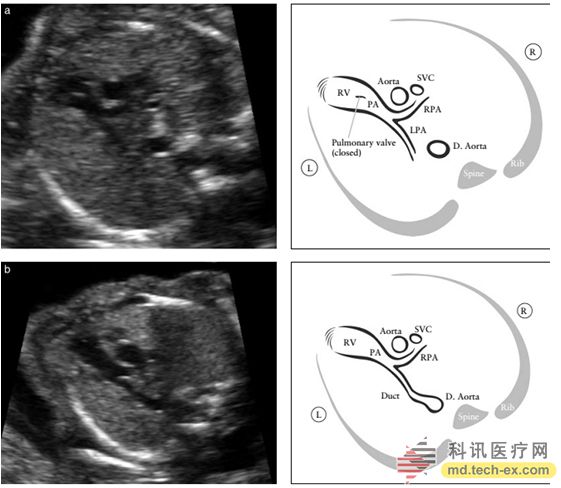
Figure 4 shows the right ventricular outflow tract (RVOT) section. This section shows the large blood vessels emanating from the right ventricle. Normally, this blood vessel spans the aorta, which helps to identify it as a pulmonary artery. The pulmonary valve is not thick and open and closed freely. Figure a shows that the pulmonary artery bifurcation enters the left and right lungs. The pulmonary valve is closed. Figure b, which is an ultrasound section closer to the cephalic side, showing the pulmonary artery, right pulmonary artery, and arterial catheter.
Three-vessel tracheal section
From the left to the right, the trivascular tracheal section is the transverse arch of the arterial catheter, the transverse arch of the aorta, and the short axis of the superior vena cava. The tracheal cross section is visible in front of the superior vena cava. The trachea usually appears as a small liquid dark area on the image, surrounded by high echoes. Both the transverse arch of the catheter and the transverse arch of the aorta are on the left side of the trachea and form a "V" shape when converging at the descending aorta (Fig. 5). The diseases that can be detected by the tri-vascular tracheal section include aortic coarctation, aortic arch dislocation, right aortic arch, right ventricular double outlet, double aortic arch, and main pulmonary artery window.
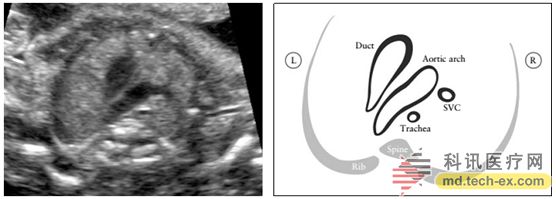
Figure 5 shows the three-vessel trachea (3VT) section, which shows the transverse arch of the aorta and its relationship to the trachea. Under normal circumstances, the aortic arch and the arterial catheter arch are located on the left side of the trachea, and the two are arranged in a "V" shape.
Color Doppler
The color flow map helps identify different heart structures and can also display abnormal blood flow. It is also an effective tool for identifying cardiac structures in obese patients, and it can increase the detection rate of major CHD in low-risk pregnant women. The best color Doppler setup involves the use of a smaller color frame (region of interest) because it has a large impact on the frame rate, proper pulse repetition frequency, low color afterglow, and sufficient gain to show the valve and blood vessels. Blood flow in.
Fetal echocardiography
Echocardiography should be performed on the fetus if the CHD is suspected, or if the above-mentioned four-chamber view and outflow tract are not available at the time of examination, or if the CHD is at high risk.
Other ultrasound techniques can also be applied to fetal heart tests, but are not recommended as routine examinations. For example, Doppler ultrasound imaging can measure blood flow velocity or identify abnormal blood flow between the valves and the heart chamber. M-mode ultrasound is also important for analyzing cardiac rhythm, ventricular function, and myocardial wall thickness. New technologies are becoming more widely used, such as tissue Doppler, and volumetric ultrasound (3D/4D/STIC) can also provide more information on the anatomy and function of the fetal heart. 4D fetal echocardiography can help diagnose complex cardiac defects, including condylar arterial malformations, aortic arch abnormalities, and abnormal pulmonary venous return. Other ultrasound methods, such as speckle tracking, are currently used primarily in the research phase, but may be an important clinical tool for evaluating fetal heart function.
Source: Chinese Obstetrics and Gynecology Online
Seeding Machine,Seed Drill,Seed Planter,Drum Seeder
Taizhou Yingtian Agricultural Machinery Manufacturing Co., Ltd. , https://www.sakuradaagc.com